A Prescription for Quebec’s Doctor Shortage

Economic Note presenting efficient ways to increase access to health care for the Quebec population
The shortcomings of health care systems across Canada have been thrown into stark relief by the pandemic, with surgery backlogs making headlines again of late. A lack of physicians and the absence of competition between private and public providers is undermining access to care. This publication proposes several ways of improving access to health care, including expanding the role of independent providers and increasing the number of doctors in Quebec. For this to happen, however, the College of Physicians and the government will have to end their intimate connection that is harming Quebecers.
 Related Content
Related Content
 |
 |
 |
| Quebec’s ailing health-care system (Financial Post, May 31, 2022) |
This Economic Note was prepared by Krystle Wittevrongel, Public Policy Analyst at the MEI, and Maria Lily Shaw, Economist at the MEI. The MEI’s Health Policy Series aims to examine the extent to which freedom of choice and entrepreneurship lead to improvements in the quality and efficiency of health care services for all patients.
Over the past couple of years, the shortcomings of Canada’s provincial health care systems have been made abundantly clear, coast to coast to coast. Given our poor performance internationally in terms of health care resources (despite consistently high health spending), our mediocre crisis response was unfortunately no surprise.(1) Yet shortages, waitlists, inaccessible services, and other structural weaknesses are nothing new; our systems have been threadbare for decades. The COVID-19 pandemic merely shone a spotlight on their meagre capacity, which can no longer be ignored.
In order to avoid falling back into old habits, Quebec should include the private sector in the provision of health care services. In fact, it should not only include, but encourage the development of independently-owned clinics and hospitals by easing the administrative barriers currently in force. Such additional facilities could help shorten waitlists for surgeries and alleviate the perpetual pressure in the government-run health system.
Another obstacle to the development of a system of private facilities, but also to the proper functioning of the public system, however, is the lack of physicians in the province. This publication thus looks to present efficient ways to increase the number of doctors in Quebec in order to ensure proper staffing in all facilities.
Where Things Stand
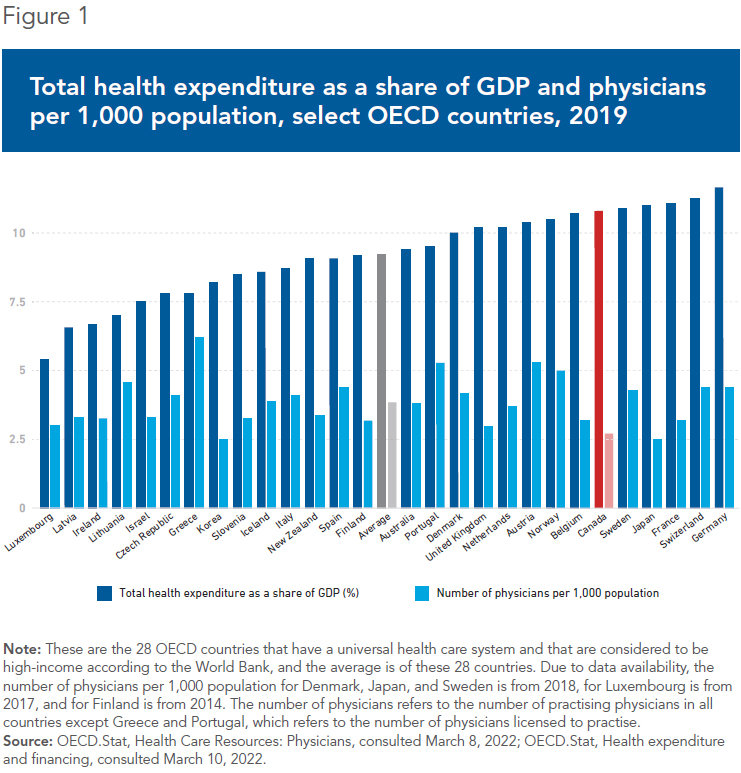
The supply of doctors is one measure of a system’s capacity, and the number of physicians in Canada is consistently lower than the OECD average.(2) In 2019, the OECD average of 3.8 physicians per 1,000 was 41% higher than Canada’s 2.7 physicians per 1,000.(3) Actually, when compared with other high-income OECD countries that have universal taxpayer-funded systems, Canada regularly ranks near the bottom for physicians per capita.(4)
In its 2021 election platform, the party in power in Ottawa pledged another $3.2 billion to hire more health care workers, including doctors.(5) However, at 10.8% of GDP in 2019, our spending on health care is already higher than most other high-income OECD countries with universal taxpayer-funded systems(6) (see Figure 1). This makes the doctor shortage even more puzzling, and seriously undermines the notion that throwing more money at the problem is a viable solution.
There are five million Canadians across the country without a family doctor.(7) As a result of this shortage, timely access to care is a serious challenge, especially in Quebec. In 2021, 69% of Quebecers were concerned about access to health services,(8) and rightly so—nearly one in five Quebecers is currently without a family doctor,(9) and the wait to get one averages 599 days in the province.(10)
Quebec struggles to provide adequate access to primary care, as indicated by the percentage of the population without access to a primary health care provider, which has consistently been higher than all other provinces in recent years (see Figure 2). This is in spite of the province spending over $47 billion(11 on its health care system in 2019, before COVID. At 10.2% of GDP,(12) Quebec spent as much as the Netherlands in 2019, but had a m)ere 2.5 physicians per 1,000 compared to 3.7 in the Netherlands.(13) This is a clear indication of Quebec’s inefficient use of resources, as are lengthy waitlists for specialists and surgeries.(14)

The lack of access is a serious concern, as primary care is an important resource for chronic disease prevention and management.(15) Studies conducted among OECD countries have shown that stronger primary care systems are associated with better population health outcomes such as lower mortality rates,(16) decreased rates of hospitalizations for ambulatory care,(17) reduced avoidable emergency room use and hospitalizations,(18) and higher infant birth weight and life expectancy,(19) not to mention lower system costs.(20) With a population that is aging as fast as Quebec’s,(21) it would be irresponsible to leave the shortage of doctors in the province unaddressed.
How Did We Get Here?
There are several legislative, regulatory, and administrative factors that contribute to the shortage of physicians in Quebec. First, medical school quotas in the province greatly limit the capacity to increase the number of practising doctors. While authorities have announced an increase in the number of students that can be admitted into medical programs in the years to come,(22) for the 2020/21 school year, Quebec’s four medical faculties admitted only 966 students while rejecting 9,553 others.(23) With such a low admission rate, the province will have at most 0.11 new doctors per 1,000 population once the 2020/21 cohort graduates, assuming every single one of the students does graduate from medical school and begin their practice in Quebec.(24)
The accreditation process is also particularly burdensome in Quebec, which makes the province less attractive to foreign medical school graduates or physicians from elsewhere in Canada. Indeed, Quebec’s proportion of foreign-trained physicians has been decreasing over the past two decades, and stood at just 8.2% in 2020, the lowest rate in the country, compared to a Canadian average of 25.7%(25) (see Figure 3).
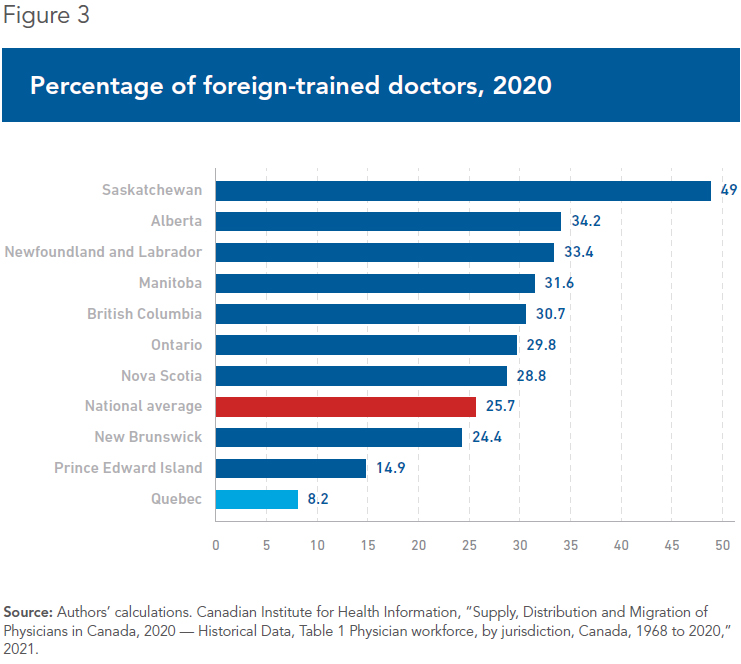
This low ratio is all the more surprising when considering the fact that Quebec has had an agreement with France since 2008 that recognizes the training and licenses acquired for various professions, including nurses and doctors.(26) However, the Quebec-France agreement is severely limited by bureaucracy, and hundreds of qualified French physicians are routinely denied the right to practise in Quebec.(27) For example, in 2016, only 44% of French doctors who applied for a license were granted one.(28) In addition, Quebec doctors in France obtain a permit and begin practising in less than two months, whereas for French doctors, if successful, the process often takes more than two years.(29)
Quebec is not a destination for doctors from other provinces, either. In fact, over the past twenty years, only six years saw more doctors moving to Quebec from other provinces rather than the other way around.(30) Research shows that physicians’ interprovincial migration decisions can be grouped into a number of categories: personal characteristics, considerations pertaining to professional practice, family concerns, level of compensation, and community characteristics.(31) The bureaucratic hassle of licensing and accreditation is a significant factor that impacts the mobility of physicians.(32)
So, not only is Quebec not attracting enough foreign-trained physicians; it is also not attracting physicians from other provinces, despite a level of remuneration in 2018/2019 roughly equal to the Canadian average.(33) Therefore, the low number of new medical school graduates joining the health care system is not supplemented enough by the arrival of doctors from other countries or from other provinces.
Moreover, like the population, the pool of practising doctors is aging. Indeed, over the past ten years, an average of 14.5% of physicians in Quebec were older than the traditional retirement age of 65.(34) A survey by the College of Family Physicians of Canada reported that 32.3% of physicians aged 65-74 planned on retiring within two years, as well as 35.4% of those over the age of 75.(35) Given the age distribution of physicians in the province, Quebec could be looking at a loss of approximately 1,083 doctors by 2024, representing more than an entire medical school cohort at current admission rates.(36)
There is also a lack of succession in family medicine, exemplified by an increase in unfilled family residency spots in the province.(37) In fact, since 2013, there have been 400 unfilled positions across the province.(38)
But how many doctors do we need? Even the Canadian Medical Association does not know the answer.(39) To reach the 2019 OECD average of 3.8 physicians per 1,000 population from its current 2.5, Quebec would need to increase the pool of physicians by approximately 10,135 overnight.(40) Considering the current size of Quebec’s medical school cohorts, the low rate of entry of medical professionals from other jurisdictions, and the age distribution of doctors coupled with the expected retirement rate, at the current pace it would take Quebec 37 years to reach the 2019 OECD average(41) (see Figure 4).

What Can Be Done? First, Make Better Use of Existing Resources
Quebec needs to increase access to health care for its residents. In addition to allowing mixed practice and expanding the participation of private facilities in the provision of care,(42) one of the simplest things to do in the short term is to make better use of existing health care resources. This can be accomplished through the delegation of more tasks and procedures to Specialized Nurse Practitioners (SNP) and pharmacists, both of which have medical training that can approach that of doctors in certain regards.(43) This will free up doctors to treat more complex cases or take on new patients.
Recent legislative changes within the province of Quebec have expanded the scope of practice of SNPs to include the diagnosis of certain diseases, the prescription of some diagnostic tests, performing some medical procedures (sutures, joint infiltration, etc.), and the prescription and administration of certain medications, among other things.(44) The amendments also rendered SNPs autonomous, so they are no longer required to continuously work in partnership with a physician.(45) These changes allow SNPs to provide more comprehensive care to patients, many of whom would have otherwise occupied a physician’s time.
These are welcome additions to SNPs’ scope of practice, but more could be done regarding the treatment of mental health problems, which is reserved exclusively to nurse practitioners specialized in mental health, thus limiting the practice of SNPs of other specialties when evaluating these problems. For example, a nurse practitioner specialized in primary care cannot act independently with her patient presenting with symptoms related to a diagnosis of depression or anxiety. These mental health issues are increasingly common in the population, and services in this field are lacking.
Considering that the rate of increase of these professionals far outpaces the growth in the number of physicians—over the past decade, there has been a 465% increase in the number of active SNPs in Quebec(46)—making full use of these health professionals is a must. Doctors, though, have historically resisted the increased autonomy of SNPs.(47)
There is also an abundant supply of pharmacists in Quebec whose scope of practice can include tasks that occupy a doctor’s time. With 1.1 per 1,000 population, there are more pharmacists practising in the province than in many of the other high-income taxpayer-funded health systems.(48) Bill 31, which came into force in 2020, expanded the scope of practice of pharmacists to allow them to prescribe certain medications, administer vaccines and some other medications, and adjust and/or renew a patient’s current prescriptions, among other tasks.(49) As with SNPs, expanding the scope of practice of these highly trained and highly skilled professionals will increase front-line access to health services.
Pharmacists and physicians have different priorities when it comes to patients, and the best use of existing resources is to focus on areas of expertise. For example, drug-related issues or concerns can easily be dealt with by a pharmacist, whereas a physician’s attention should be sought for conditions requiring a clinical diagnosis.(50) As drug-related problems account for more than 10% of ER visits across the country, effective collaboration between physicians and pharmacists can reduce drug-related hospital visits.(51)
Communication is key, both for patients and providers. Patients need to know how and where to appropriately seek care, and providers need to refer appropriately and collaborate as needed. This not only has the potential to free up doctors’ time to take on the more complex medical cases and increase access to care overall, but it also provides patients with the best possible care.
Next, Increase the Supply
Ending medical school quotas is a surefire way to increase the number of doctors in the province. Since medical training takes six to eleven years to complete,(52) not counting the several years of academic training or any additional preparatory work beforehand, there is no time to waste.
Another option is to attract additional resources by reducing the profession’s barriers to entry. People move between provinces or countries for a wide range of reasons, but in deciding whether to do so, the associated costs—including processing times and administrative and regulatory hurdles to exercising one’s profession—are carefully considered. These barriers are an added cost to migration and therefore a disincentive to moving to Quebec. Easing the bureaucratic load in the accreditation process and the recognition of credentials is one way to increase the supply of doctors in the province.
Looking to other provinces for inspiration, Alberta has taken steps to increase interprovincial labour mobility with its Bill 49, passed in late 2021. This bill introduced a maximum timeline of 20 business days to recognize credentials and training from other Canadian provinces for physicians and surgeons, among other regulated professions.(53) Standardizing and streamlining processes enhances provincial labour mobility, and more skilled workers are expected. This is something Quebec should also consider, in addition to a similar removal of the barriers for foreign-trained doctors. It could start by making better use of the agreement with France and streamlining the applications of French doctors, just as France has done for Quebec applications.
Conclusion
The role of private sector care providers in Quebec must be expanded to finally improve access to health care for Quebecers. As outlined above, to address the lack of doctors and ensure proper staffing in all facilities, the government should also:
- Make the best use of existing health professionals, such as SNPs and pharmacists, to reduce the pressure on a physician’s time, therefore providing additional availability to other patients and more complex cases;
- Eliminate medical school quotas, which will increase the number of trained physicians and also allow the backlog of residency positions to resolve;
- Expand the health care workforce with foreign-trained doctors and doctors from other provinces by easing the regulatory barriers to entering the Quebec workforce.
These recommendations are tangible and concrete. In fact, they have been employed in Canada to some extent in the past. During the 1990s, the number of physicians decreased across the country,(54) and between 2003 and 2013, efforts were made to remedy this.55 A significant increase in the number of medical school admissions (48%) coupled with the integration of more foreign-trained doctors were some of the tactics employed.(56) As a result, the number of physicians in Canada grew from 2.0 physicians per 1,000 population in 2003 to 2.5 physicians per 1,000 in 2013, a 25% increase.(57)
Accessibility is one of the five principles of the Canada Health Act.(58) To meet this condition, the Quebec government should consider how to best increase the number of physicians in the province. Indeed, with 91% of Quebecers agreeing that there is a need to improve health care capacity, this should be one of its top priorities.(59)
References
- Tristin Hopper, “Why Canada’s hospital capacity was so easily overwhelmed by the COVID pandemic,” National Post, January 17, 2022.
- This is the average of the 28 OECD countries that have a universal health care system and that are considered to be high-income according to the World Bank, which are featured in Figure 1. Mackenzie Moir and Bacchus Barua, Comparing Performance of Universal Health Care Countries, 2021, Fraser Institute, 2021, pp. 4 and 6.
- OECD.Stat, Health Care Resources: Physicians, consulted March 8, 2022.
- Authors’ calculations. Between 2016 and 2019, Canada consistently ranked 26 out of the 28 countries included in Figure 1 for number of physicians per 1,000 population. Idem.
- Liberal Party of Canada, Forward. For Everyone., 2021, p. 3.
- OECD.Stat, Health expenditure and financing, consulted March 10, 2022.
- Tristin Hopper, “Why five million Canadians have no hope of getting a family doctor,” National Post, January 25, 2022.
- Nathalie de Marcellis-Warin and Ingrid Peignier, Perception des risques au Québec – Baromètre CIRANO 2021, Cirano, 2021, p. 90.
- Michelle Lalonde, “Quebec’s family doctor problem: Will Legault’s tough talk solve anything?” Montreal Gazette, November 9, 2021.
- Patrick Bellerose, “599 jours d’attente pour avoir son médecin de famille au Québec,” Le Journal de Québec, August 2, 2021.
- Authors’ calculations. For the 2019 fiscal year, in current dollars according to the inflation calculator of the Bank of Canada. Government of Quebec, Public Accounts 2019-2020: Consolidated Financial Statements of the Gouvernement du Québec, 2020, p. 20.
- Institut de la Statistique du Québec, Produit intérieur brut régional par industrie au Québec – Édition 2021, Government of Quebec, September 2021, p. 10; Government of Quebec, op. cit., endnote 11.
- OECD Data, Health, Health Resources, Health Spending, consulted March 10, 2022; Canadian Institute for Health Information, “Supply, Distribution and Migration of Physicians in Canada, 2020 — Historical Data, Table 1 Physician workforce, by jurisdiction, Canada, 1968 to 2020,” 2021; OECD.Stat, Health Care Resources: Physicians, consulted March 8, 2022.
- Maria Lily Shaw, Real Solutions for What Ails Canada’s Health Care Systems: Lessons from Sweden and the United Kingdom, MEI, Research Paper, February 2022, p. 14.
- Canadian Medical Association, “Family Medicine Profile,” August 2018, p. 4.
- James Macinko, Barbara Starfield, and Leiyu Shi, “The Contribution of Primary Care Systems to Health Outcomes within Organization for Economic Cooperation and Development (OECD) Countries, 1970-1998,” Health Services Research, Vol. 38, No. 3, May 23, 2003, pp. 846-851.
- Matthew Niti and Tse-Pin Ng, “Avoidable hospitalisation rates in Singapore, 1991- 1998: Assessing trends and inequities of quality in primary care,” Journal of Epidemiology & Community Health, Vol. 57, No. 1, 2003, p. 21.
- Leiyu Shi, “The Impact of Primary Care: A Focused Review,” Scientifica, 2012, p. 7; Mala Rao and Eva Pilot, “The missing link – the role of primary care in global health,” Global Health Action, Vol. 7, No. 1, 2014, p. 2.
- James Macinko, Barbara Starfield, and Leiyu Shi, “Quantifying the Health Benefits of Primary Care Physician Supply in the United States,” International Journal of Health Services, Vol. 37, No. 1, 2007, p. 121.
- Barbara Starfield and Leiyu Shi, “Policy relevant determinants of health: an international perspective,” Health Policy, Vol. 60, No. 3, June 2002, p. 205.
- Institut de la Statistique du Québec, “Towards a population of 10 million people in Québec by 2066,” Press release, June 17, 2021.
- Vincent Larin, “Québec augmente les admissions en médecine,” TVA Nouvelles, May 22, 2020.
- Authors’ calculations. The Association of Faculties of Medicine of Canada, Canadian Medical Education Statistics 2020, 2020, pp. 66 and 150.
- Authors’ calculations. Accounts for the growth of population from 2020 until 2031, when the 2020/21 cohort is expected to graduate at the very latest. Institut de la Statistique du Québec, Population and components of demographic growth, Québec, 1971-2021 (in French only), consulted March 10, 2022; The Association of Faculties of Medicine of Canada, Idem.
- Authors’ calculations. Canadian Institute for Health Information, op. cit., endnote 13.
- Government of Quebec, Immigration, Francisation et Intégration, Entente France-Québec sur la reconnaissance mutuelle des qualifications professionnelles, consulted March 10, 2022. For doctors and nurses, it is since 2010 and 2011 that their profession is included in the agreement. Government of Quebec, Emploi, entente Québec-France, Métiers et professions de la France encadrés par l’entente Québec-France, consulted march 10, 2022.
- Authors’ calculations. Antoine Dumas-Martin, L’Entente Québec-France et ses limites : le cas des médecins de famille, École de politique appliquée Faculté des lettres et sciences humaines, Université de Sherbrooke, 2014, p. 9; Sophie Langlois, “Le Québec ferme la porte à près de 200 médecins français,” Radio-Canada, April 5, 2020.
- Authors’ calculations. Sophie Langlois, Idem.
- Idem.
- Between 2001 and 2020. Canadian Institute for Health Information, op. cit., endnote 13.
- Haizhen Mou and M. Rose Olfert, “Inter-Provincial Migration Intentions of Family Physicians in Canada: The Roles of Income and Community Characteristics,” Healthcare Policy, Vol. 11, No. 2, November 2015, pp. 60-61.
- Michael Gorman, “Doctors want provincial barriers broken, call for national licensing system,” CBC News, August 23, 2018.
- In 2018/2019, the average gross clinical payment per physician in Canada was $347,000, and in Quebec for that same period it was $345,000. Canadian Institute for Health Information, Physicians in Canada, 2019: Summary report, 2020, p. 26.
- Authors’ calculations. The average is based on the proportion of physicians over the age of 65 for the years 2011-2020. Canadian Institute for Health Information, op. cit., endnote 13.
- This is based on the 2007 National Physician Survey by the College of Family Physicians of Canada. Raymond W. Pong, Putting Away the Stethoscope for Good? Toward a new Perspective on Physician retirement, Canadian Institute for Health Information, March 2011, p. 65.
- Authors’ calculations. Canadian Institute for Health Information, op. cit., endnote 13; The Association of Faculties of Medicine of Canada, op. cit., endnote 23.
- Maude Laberge and Myriam Gaudreault, “Promoting access to family medicine in Québec, Canada: Analysis of bill 20, enacted in November 2015,” Health Policy, Vol. 123, No. 10, October 2019, p. 904.
- Davide Gentile and Daniel Boily, “Orphelin de médecin, pris en charge par une infirmière,” Radio-Canada, February 23, 2022.
- Monica Kidd, “Canada doesn’t know how bad its doctor shortage is, let alone how to fix it,” National Post, October 27, 2021.
- Authors’ calculations. Canadian Institute for Health Information, op. cit., endnote 13.
- Authors’ calculations. This is assuming the current average annual growth rate of 2% over the past 20 years for the number of physicians remains constant, as well as the average annual growth rate over the past 20 years of 1% for the total population of Quebec. Canadian Institute for Health Information, Idem.
- Marcel Boyer and Julie Frappier, “Medical Specialists in Quebec: How to Unlock the Reserve Supply,” MEI, Economic Note, April 2009, pp. 2-4; Maria Lily Shaw, op. cit., endnote 14, pp. 53-54.
- Peter St. Onge and Maria Lily Shaw, For a Strong and Resilient Post-COVID Health Care System – Reforms to Expand Surge Capacity, MEI, Research Paper, December 2020, pp. 39-40.
- Government of Quebec, “Regulation respecting specialized nurse practitioners,” September 15, 2021, p. 8; National Assembly of Quebec, “Bill 43 – An act to amend the Nurses Act and other provisions in order to facilitate access to health services,” Government of Quebec, 2019, p. 5; Martine Maillé, Specialized Nurse Practitioners and Their Practice, Ordre des infirmières et infirmiers du Québec, February 19, 2021, p. 25.
- Irene Sarasua and Christina Kozakiewicz, “New legislation brings big changes for Quebec nurse practitioners and patients,” McGill Faculty of Medicine and Health Sciences, Ingram School of Nursing, February 11, 2021.
- As of March 31, 2021, there were 842 SNPs in the province. Daniel Marleau, Rapport statistique sur l’effet infirmier et la relève infirmière du Québec, 2020-2021, Ordre des infirmières et infirmiers du Québec, 2021, p. 14.
- Jocelyne Richer, “ ‘Super nurses’ gain powers, but look for more autonomy,” Montreal Gazette, February 14, 2018.
- Authors’ calculations, based on 9,460 pharmacists in Quebec in 2019. Compared with the countries listed in Figure 1. At 1.1 per 1,000, both Quebec and Canada are higher than the average of 1.0 per 1,000. OECD.Stat, Health Care Resources: Pharmacists, consulted March 10, 2022; Canadian Institute for Health Information, Pharmacists in Canada, 2019 — Data Tables, 2020.
- National Assembly of Quebec, op. cit., endnote 44, p. 2.
- Eugene Y. H. Yeung, “Pharmacists Becoming Physicians: For Better or Worse?” Pharmacy, Vol. 6, No. 3, 2018, p. 3.
- Cara Tannebaum and Ross T. Tsuyuki, “The expanding scope of pharmacists’ practice: Implications for physicians,” Canadian Medical Association Journal, Vol. 185, No. 14, October 2013, p. 1229.
- Université Laval, Faculté de Médecine, Programmes d’études, Résidences (études médicales postdoctorales), consulted March 15, 2022.
- Government of Alberta, “Bill 49: Labour Mobility Act,” October 2021; Government of Alberta, “Bill 49: Labour Mobility Act occupations,” October 2021, p. 1.
- Benjamin TB Chan, From Perceived Surplus to Perceived Shortage: What Happened to Canada’s Physician Workforce in the 1990s? Canadian Institute for Health Information, June 2002, p. 15.
- Andrei V. Malko and Vaughn Huckfeldt, “Physician Shortage in Canada: A Review of Contributing Factors,” Global Journal of Health Science, Vol. 9, No. 9, June 1st, 2017, p. 68.
- Association of Faculties of Medicine of Canada, Canadian medical education statistics, 2014, as cited in Andrei V. Malko and Vaughn Huckfeldt, Idem.
- Authors’ calculations. Canadian Institute for Health Information, op. cit., endnote 13.
- Government of Canada, Canada Health Act, Minister of Justice, December 12, 2017, p. 5.
- Ipsos, “Healthcare in Canada 2021,” Poll conducted on behalf of the MEI, November 2021, p. 9.

