Improving Access to Care by Expanding the Role of Pharmacists
While Quebec’s public health care system struggles to respond adequately to the needs of patients, and the cost of the system continues to rise rapidly, expanding the role of pharmacists in offering front-line services is without a doubt a step in the right direction. These increased responsibilities are likely to improve patients’ access to care and lead to savings, which the public system desperately needs.
Media release : A greater role for pharmacists to reduce health care wait times: The reform does not go far enough
 Related Content
Related Content
 |
 |
 |
| Pharmacists can help reduce health-care wait times, if we let them (Montreal Gazette, May 1st, 2015) | Debate (in French) with Yanick Labrie (À la une, ARGENT business news network, April 30, 2015)
Interview (in French) with Yanick Labrie (Mario Dumont, LCN news network, April 30, 2015) |
Improving Access to Care by Expanding the Role of Pharmacists
In December 2011, the Quebec government adopted Bill 41 for the purpose of expanding the scope of practice for pharmacists and thereby improving patients’ access to care. In principle, the legislative change authorized pharmacists to offer seven new pharmaceutical services, including renewing or adjusting prescriptions, substituting drugs in cases of supply shortages, and prescribing drugs for minor ailments when no diagnosis is required. Implementation of the reform has been delayed, however, and these new consultations are still not on offer, due to the stalled negotiations between the government and the Association québécoise des pharmaciens propriétaires regarding their remuneration.(1)
While Quebec’s public health care system struggles to respond adequately to the needs of patients, and the cost of the system continues to rise rapidly, expanding the role of pharmacists in offering front-line services is without a doubt a step in the right direction. These increased responsibilities are likely to improve patients’ access to care and lead to savings, which the public system desperately needs.
Accessing Care Remains as Difficult as Ever
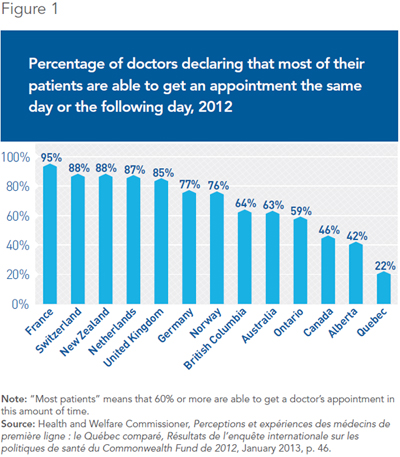
The difficulty of accessing front-line care is the Achilles heel of the Quebec health care system. Despite the ever-increasing resources devoted to it for the past twenty-five years, wait times for required care remain as much of a concern as ever. Among all the provinces, it is in Quebec that we find the longest delays before receiving an appointment with a primary care physician.(2)
According to survey data from the Health and Welfare Commissioner, just 22% of general practitioners report that most of their patients can get an appointment the same day or the following day when they need one. In comparison, that figure is 59% for Ontario doctors, and over 75% for doctors in many other countries in Europe and elsewhere(3) (see Figure 1). This situation is all the more worrisome given that Quebec has 15% more family doctors than Ontario does as a proportion of population.(4)
When it comes to accessing medical services evenings and weekends, the situation in Quebec is hardly any more encouraging. Over 60% of Quebec patients believe that it is “somewhat difficult” or “very difficult” to have access to medical care outside of normal office hours.(5) Short on options, many patients have no choice but to visit a hospital emergency room. In 2012-2013, emergency room overcrowding had gotten so bad that the average wait time was 9 hours, nearly two hours longer than it was a decade ago.(6)
These access difficulties stem in large part from the inability of a sizable portion of the Quebec population to find a family doctor. In 2013, nearly one in four Quebec adults still had no regular doctor, the highest proportion in the country.(7)
The Benefits of Turning to Pharmacists
At the moment, a high percentage of Quebec patients visit hospital emergency rooms or consult general practitioners in doctors’ offices or clinics for benign health problems requiring relatively simple medical interventions. According to a recent report from the Health and Welfare Commissioner, over 60% of hospital emergency room visits are for minor health conditions that could be better treated elsewhere.(8) Needless to say, these visits monopolize substantial amounts of medical resources and a non-negligible portion of doctors’ time.
As they are far more accessible evenings and weekends than doctors, pharmacists are ideally positioned to take care of many patients grappling with minor ailments. By turning to pharmacists for help, many patients will avoid the long wait times to see a doctor in the public system and will enjoy faster access to the care they need. Entrusting pharmacists with more responsibilities is also likely to reduce current demands on other, more expensive health care resources such as doctors and hospital emergency rooms. This will allow doctors to devote more time to cases that are more urgent or complex, entailing a more efficient use of resources and of public funds.
Internationally, pharmacists are increasingly integrated into front-line services and collaborate with doctors and other health professionals in order to improve the efficiency of the health care system and access to care. In the United Kingdom, New Zealand, and the United States, among others, the authorization to prescribe drugs and to renew prescriptions has been in effect for several years.(9) The resulting benefits are well documented.
In England, pharmacists have had greater authority to offer pharmaceutical services since 2005, including that of prescribing drugs in certain circumstances. In recent years, many pharmacies have implemented a variety of programs to take charge of minor ailments. According to a recent evaluation, these new services offered by pharmacists have freed up working hours for many general practitioners and generated savings of around 23 million Canadian dollars a year for the country as a whole. The majority of patients (58.1%) would have consulted their family doctor if the service had not been offered by pharmacists, which would in all likelihood have resulted in extra costs for the health care system.(10) In addition to these savings, however, it is reasonable to think that the most important benefits accrue to patients themselves, who have faster access to the care they need.
Several countries have also created programs designed to delegate responsibilities to pharmacists when it comes to following patients suffering from chronic diseases.(11) Giving pharmacists a greater role to play in reviewing and managing medications has led to improved treatment adherence and to reduced health risks and avoidable hospital admissions. These services have brought substantial benefits for patients suffering from chronic diseases like hypertension, asthma, and diabetes.(12)
In Canada, it is estimated that over two million people suffer from poorly controlled hypertension. Setting up a program to manage hypertension in community pharmacies would not only lead to lower blood pressure levels for many patients, but would likely generate substantial savings for the public health care system. The potential savings are evaluated at $70 million for Canada as a whole, even if only one in four patients benefits from the program.(13)
A Greater Role for Pharmacists in the Other Provinces
Conscious of the benefits that the services of pharmacists can bring in terms of improving access to front-line care, the governments of several provinces have started in recent years to delegate certain tasks that were traditionally the responsibility of doctors. Pharmacists are increasingly being allowed to prescribe drugs to treat minor conditions, to renew prescriptions, and to set up vaccination clinics, among other services (see Table 1).

In 2007, Alberta became the first province to allow pharmacists to prescribe drugs for the treatment of minor ailments. Several provinces have since followed suit, including Saskatchewan, Manitoba and the Atlantic provinces. Since February 2012, pharmacists in Saskatchewan are remunerated for the prescription of drugs to treat various health conditions not requiring a doctor’s diagnosis. A recent evaluation found a very high level of customer satisfaction, both in terms of improving health and in terms of the quality of the services delivered by the pharmacist. Only 5.6% of patients said that a doctor would have been better able to provide this service.(14)
In every province except for Quebec and Manitoba, pharmacists also offer medication review and management services, which are covered publicly. The fees paid to pharmacists vary from one province to the next according to the scope of services provided and the kinds of diseases patients are suffering from.
In Ontario, the MedsCheck program has since 2007 offered certain patients suffering from a chronic disease the possibility of obtaining a complete individual consultation with a pharmacist once a year in order to optimize the effectiveness of their medication and encourage adherence. The government pays the pharmacist’s fee, which varies between $60 for a basic review in pharmacy and $150 for such a service provided in the home.(15) Given the program’s success and popularity, the Ontario government decided to expand it in 2010 in order to make it accessible to a larger number of patients.(16)
For a few years now, the governments of seven provinces have also remunerated pharmacists for administering vaccines to prevent certain infectious diseases, including the seasonal flu.(17) These provinces all have higher influenza immunization rates than Quebec, where less than a quarter of the population receives the vaccine.(18) In Ontario, the program set up in 2012 quickly enjoyed substantial support from the population. In 2013-2014, over 765,000 Ontarians received the flu vaccine in a pharmacy.(19) When surveyed, 99% of Ontario patients report that they would recommend pharmacist vaccination to their friends and family members.(20)
Conclusion
At the moment, even taking into account the prospective implementation of the reform authorizing pharmacists to provide new professional services, Quebec still trails the other Canadian provinces. Additional responsibilities could be entrusted to pharmacists, as has been done in these other provinces, notably Alberta and Ontario.
Pharmacists are the health professionals that are most accessible to the population.(21) The scientific literature leaves little doubt about the benefits that can result from expanding their role within the health care system. Several studies confirm that the implementation of reforms entrusting pharmacists with greater responsibilities in other countries has helped improve patient access to care and the quality of that care, all while lightening the load for the public health care system.
While the forthcoming implementation of the reform will be welcome, the government’s decision not to remunerate some of the newly authorized professional services and to forbid pharmacists from charging a fee for these services runs the risk of discouraging pharmacists from providing them. By proceeding in this manner, the reform could fail to achieve its main objective, which is to improve patients’ access to care.
This Economic Note was prepared by Yanick Labrie, Economist at the Montreal Economic Institute and holder of a master’s degree in economics (Université de Montréal). The MEI’s Health Care Series aims to examine the extent to which freedom of choice and private initiative lead to improvements in the quality and efficiency of health care services for all patients.
* * *
References
1. See among others Amélie Daoust-Boisvert, “Québec impose ses conditions aux pharmaciens,” Le Devoir, November 27, 2014, p. A3. It should be noted that despite the recent adoption of Bill 28 on April 21, negotiations on this issue are ongoing between the government and the Association québécoise des pharmaciens propriétaires.
2. Health and Welfare Commissioner, Perceptions et expériences de soins de la population : le Québec comparé, Résultats de l’enquête internationale sur les politiques de santé du Commonwealth Fund de 2013, January 2014.
3. Health and Welfare Commissioner, Perceptions et expériences des médecins de première ligne : le Québec comparé, Résultats de l’enquête internationale sur les politiques de santé du Commonwealth Fund de 2012, January 2013, p. 46.
4. Claude E. Forget, “The Case of the Vanishing Québec Physicians: How to Improve Access to Care,” C.D. Howe Institute, Commentary No. 410, May 2014, p. 5.
5. Health and Welfare Commissioner, op. cit., footnote 2, p. 27.
6. Health and Welfare Commissioner, Les urgences au Québec : évolution de 2003-2004 à 2012-2013, September 2014, pp. 14-15 and 50; author’s calculations based on data regarding average durations for ambulatory visits and those on stretchers.
7. Statistics Canada, CANSIM Table No. 105-3024: Population reporting a regular family physician, household population aged 15 and over, Canada, provinces and territories, 2013.
8. La Presse canadienne, “60 % des visites à l’urgence sont inutiles,” Le Devoir, September 18, 2014.
9. Cara Tannenbaum and Ross T. Tsuyuki, “The Expanding Scope of Pharmacists’ Practice: Implications for Physicians,” Canadian Medical Association Journal, Vol. 185, No. 14, August 2013, pp. 1228-1232.
10. W. Baqir, T. Learoyd, A. Sim and A. Todd, “Cost Analysis of a Community Pharmacy ‘Minor Ailment Scheme’ Across Three Primary Care Trusts in the North East of England,” Journal of Public Health, Vol. 33, No. 4, 2011, pp. 551-555; Bank of Canada, “Annual Average Exchange Rates,” Financial Markets Department, March 2015.
11. Elias Mossialos et al., “From ‘Retailers’ to Health Care Providers: Transforming the Role of Community Pharmacists in Chronic Disease Management,” Health Policy, 2015 (forthcoming).
12. See among others Yazid N Al Hamarneh et al., “Pharmacist Intervention for Glycaemic Control in the Community (the RxING Study),” BMJ Open, Vol. 4, No. 3, 2013; Valérie Santschi, Ross T. Tsuyuki and Gilles Paradis, “Evidence for Pharmacist Care in the Management of Hypertension,” Canadian Pharmacist Journal, Vol. 148, No. 1, 2015, pp. 13-16; George Adulin and Soheyla Mahdavian, “The Effectiveness of Pharmacist Interventions on Asthma Management: A Systematic Review,” Journal of Asthma and Allergy Educators, Vol. 3, No. 6, 2012, pp. 264-273.
13. Sherilyn K. D. Houle et al., “Effect of a Pharmacist-Managed Hypertension Program on Health System Costs: An Evaluation of the Study of Cardiovascular Risk Intervention by Pharmacists – Hypertension (SCRIP-HTN),” Pharmacotherapy, Vol. 32, No. 6, 2012, pp. 527-537.
14. Kerry Mansell et al., “Evaluating Pharmacist Prescribing for Minor Ailments,” International Journal of Pharmacy Practice, Vol. 23, 2015, pp. 95-101.
15. Canadian Foundation for Pharmacy, “Fees and Claims Data for Government-Sponsored Pharmacist Services, by Province,” October 2014.
16. Ontario Ministry of Health and Long-Term Care, MedsCheck Program Expands: McGuinty Government Ensuring More One-on-One Pharmacist Consultations, News release, November 8, 2010.
17. Canadian Foundation for Pharmacy, op. cit., footnote 15.
18. Statistics Canada, CANSIM Table No. 105-0501: Health indicator profile, annual estimates, by age group and sex, Canada, provinces, territories, health regions and peer group, 2013.
19. Sony Poulose et al., “Pharmacist-Administered Influenza Vaccine in a Community Pharmacy: A Patient Experience Survey,” Canadian Pharmacist Journal, Vol. 148, No. 2, 2015, pp. 64-67.
20. John Papastergiou et al., “Community Pharmacist-Administered Influenza Immunization Improves Patient Access to Vaccination,” Canadian Pharmacist Journal, Vol. 147, No. 6, 2014, pp. 359-365.
21. On this topic, see Yanick Labrie, Chapter 2: “Pharmacies in Canada: Accessible Private Health Care Services,” in The Other Health Care System: Four Areas Where the Private Sector Answers Patients’ Needs, Research Paper, Montreal Economic Institute, March 2015, pp. 17-23.

